Leishmaniasis is a parasitic disease that is found in parts of the tropics, subtropics, and southern Europe. It is classified as a Neglected Tropical Disease (NTD). Leishmaniasis is caused by protozoan Leishmania parasites from over 20 Leishmania species which are transmitted by bites from infected female phlebotomine sandflies. Over 90 sandfly species are known to transmit Leishmania parasites.
 Sand flies are responsible for the spread of Leishmaniasis, caused by the obligate intracellular protozoa of the genus Leishmania.
Sand flies are responsible for the spread of Leishmaniasis, caused by the obligate intracellular protozoa of the genus Leishmania.
There are 3 forms of leishmaniases – visceral (also known as kala-azar and the most serious form of the disease), cutaneous (the most common), and mucocutaneous. Almost 70 animal species, including humans, have been found to be natural reservoir hosts for Leishmania parasites. This pathogen’s ability to remain in the host and maintain a chronic infection depends on its evasion of the host immune system.
Like other pathogens, Leishmania has also evolved smart ways to escape the host immune system. One such mechanism targets macrophages. Ideally, macrophages fight against Leishmania, however, they are the primary host cells targeted by the parasite for survival and proliferation. This is possible due to the cell surface lipophosphoglycan that enables Leishmania binding to mannosyl/fucosyl receptors on the macrophage. Other proteins such as glycosylinositol phospholipid and GP63 also play similar roles.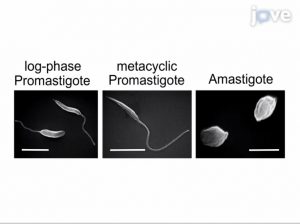
Sarkar, A. et. al, demonstrated how Leishmania parasites inside macrophages can be assessed. The authors developed a technique to observe the intracellular development of Leishmania in bone marrow-derived macrophages. They also analyzed different forms of Leishmania using Scanning Electron Micrography.
Another way by which Leishmania compromises the immune system is by altering functions of immune cells. The parasites can bind to Toll-like receptors (TLRs), which are expressed on the surface of cells involved innate immunity. This TLR-binding either alters cytokine induction by negatively regulating TLR2 or accelerates expression of factors via TLR signaling, which facilitates the establishment of infection. In 2015, Layoun, A, et al. described gene expression analysis of murine macrophages upon TLR stimulation. In this study, isolated macrophages were challenged with different TLRs agonists, followed by a PCR-based estimation of gene expression.

While understanding how leishmaniasis occurs is important; its diagnosis and treatment are also equally important. Traditionally, serological tests and clinical signs with parasitological analysis have been sufficient for diagnosis. However, this is only true for visceral leishmaniasis. Such studies have limited value for cutaneous and mucocutaneous leishmaniasis diagnoses. Leishmaniasis treatment would depend on many factors such as disease type, parasite species, geographic location, etc. According to WHO, Leishmaniasis is a curable disease. The treatment requires an immunocompetent system since medicines do not remove the parasite from the body, hence there is a risk of relapse in case of immunosuppression. Since there are no vaccines or drugs which prevent the infection, the best way is to protect oneself from sand fly bites by using repellents and minimizing exposure of the skin.

